Antibiotic Selection in Pyoderma
Growing antibiotic resistance has complicated the treatment of bacterial skin conditions. Here’s what to consider when making therapeutic decisions for your patients.
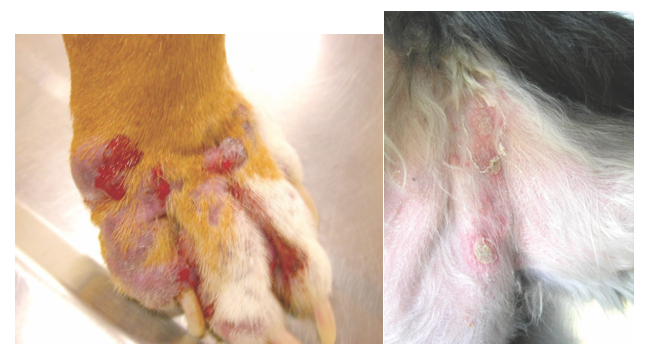
(Left) Draining tracts on the foot of a dog with pyoderma. (Right) Epidermal collarette.
Bacterial pyoderma is one of the most commonly diagnosed dermatologic diseases in dogs. Although β-lactam antibiotics such as cephalexin were once effective in treating pyoderma, the growing emergence of resistant bacteria, particularly methicillin-resistant Staphylococcus, has made treatment of this condition much more complicated. At the 2018 Midwest Veterinary Conference in Columbus, Ohio, Paul B. Bloom, DVM, DACVD, DABVP (Canine & Feline), discussed the diagnosis and treatment of pyodermas, with a particular focus on using a bacterium’s minimum inhibitory concentration (MIC) to select the proper antibiotic.
RELATED:
- New Findings on the Pathogenesis of Canine Demodicosis
- ACVC 2017: Understanding Skin Disease in Cats
The frequency of antibacterial resistance in both human and veterinary medicine has been increasing. This increased resistance heightens the risk of spreading antibacterial resistance genes between animals and people, said Dr. Bloom, an adjunct assistant professor in the Department of Small Animal Clinical Sciences at Michigan State University College of Veterinary Medicine and a practitioner at the Allergy, Skin and Ear Clinic for Pets in Livonia, Michigan. Previous studies, for example, have reported the transfer of drug-resistant Escherichia coli, methicillin-resistant Staphylococcus aureus (MRSA), and methicillin-resistant Staphylococcus pseudintermedius (MRSP) between pets and people.1-4
Characterizing Pyodermas
Pyodermas are typically caused by a staphylococcus. In recent years, methicillin-resistant Staphylococcus—MRSA, MRSP, MRSS (schleiferi), MRSI (intermedius)—has been identified increasingly in canine pyodermas.
Superficial bacterial folliculitis (SBF), a superficial pyoderma, is characterized by such clinical signs as variable pruritus, multifocal alopecia, follicular papules or pustules, and epidermal collarettes. In addition, serous serocelluar crusts can be found on the trunk and abdomen, and in axillary regions. Short-haired breeds with SBF may present with a moth-eaten appearance. Notably, cocker spaniels with SBF can present with vegetative plaques that can be mistaken for seborrheic plaques.
Deep pyodermas are characterized typically by nodules, hemorrhagic bullae, and serosanguineous to purulent draining tracts. Deep pyoderma lesions can be found on the nose, chin, elbows, hocks, and interdigital spaces.
Diagnosing Pyodermas
Diagnosing bacterial pyodermas requires a systematic approach, which includes obtaining a thorough history and performing a dermatologic examination.
History
Obtaining a detailed history involves asking numerous questions about a dog’s condition:
- When did the signs first occur? Have they progressed rapidly or gradually?
- Has the dog been treated previously for skin or ear disease? If yes, what was used and for how long? What was the dog’s response?
- Does the dog live indoors, outdoors, or both?
- Is the dog pruritic? If so, did the rash develop first, or did the pruritus and rash begin simultaneously?
- Compared with the first appearance of signs, is today’s clinical presentation better, worse, or about the same?
- Are there other pets living in the household? If so, do they have skin problems?
- What is the dog’s diet?
- What medication is the dog currently receiving?
Dermatologic Examination
The dermatologic examination serves to identify primary lesions (eg, papules, pustules, nodules) and secondary (eg, ulcerations, crusts) lesions, detect ectoparasites, observe evidence of self-trauma, and determine hair coat quality and skin appearance. The exam should include an impression smear of a lesion, in which infectious agents, neoplastic cells, inflammatory cells, and pemphigus foliaceus—associated acantholytic keratinocytes can be evaluated. Skin scrapings for ectoparasites and flea combing are essential parts of a dermatology minimum database.
The patient history and results of the dermatologic examination form the basis for the differential diagnosis. This list is important, given that canine pyodermas are never primary diseases and are always “due to” something, Dr. Bloom noted. Potential differentials include hypersensitivities (eg, atopy), endogenous or exogenous steroid exposure, ectoparasites, hypothyroidism, and follicular dysplasias.
It is especially important to rule out demodicosis in dogs with lesions that are consistent with SBF. In addition, the presence of pustules requires ruling out pemphigus foliaceous.
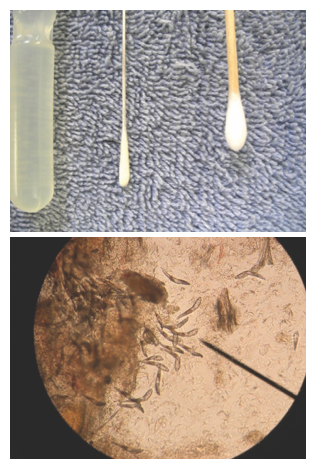
(Top) Mini-tip culturette versus standard culturette. (Bottom) Demodex mites.
Culture and Susceptibility Testing
Culture and susceptibility (C/S) testing is an important diagnostic component and is recommended for poorly responsive SBF. It is also warranted at the first visit for the following scenarios:
- Deep bacterial pyoderma with predominantly rods on cytology
- Pyoderma accompanied by systemic illness
- Recent antibiotic therapy
There are several ways to obtain samples for C/S testing. For example, mini-tip culturettes, rather than large swabs, are ideal for sampling from draining tracts and pustules. A papule, Dr. Bloom mentioned, can be sampled like a pustule in which the papule or pustule is ruptured with a needle and then the swab is touched carefully to the surface of the lesion. For patients with epidermal collarettes, he recommended swabbing just underneath the collarette’s edge. Because lesions can have bacterial strain heterogeneity, which can lead to different antibiotic susceptibilities, samples should be taken from 3 or 4 locations but all can be sampled with the same swab.
Sampling can be done while a patient is on antibiotics; to date, there is no empiric evidence to support waiting until the end of antibiotic therapy to obtain a sample for C/S testing. “When a client is there and you can do something,” Dr. Bloom emphasized, “go ahead and do it [right] then,” because clients may be too busy or may not see the importance of returning to the veterinary office for a recheck of the pyoderma, particularly if the signs have improved.
That said, if a dog is not currently on antibiotics, Dr. Bloom advised waiting until after culture results come back before starting antibiotic therapy, unless the dog has a fever or a life-threatening illness. Starting antibiotic therapy before the results come back could result in altered susceptibility patterns, thus complicating results.
The old method of C/S testing was the disk diffusion method (Kirby-Bauer method), which determines susceptibility (susceptible, intermediate, resistant) based on the zone of inhibition in a solid medium. This method, however, does not provide an accurate measure of how susceptible a bacterial strain is to a particular antibiotic.
The tube dilution method, which is quantitative, is the preferred method of C/S testing. Each test tube contains the same concentration of bacteria (105/mL) and serially increasing antibiotic concentrations (which vary among antibiotics); each tube contains double the antibiotic concentration as the previous tube. This method tells how susceptible a bacterial strain is to an antibiotic by reporting the MIC: the concentration of the first tube in which there is no visible bacterial growth. The MIC and Breakpoint
Simply having the MIC is not enough to determine which antibiotic to use to treat bacterial pyodermas. Another value—the “break-point”—is also important. The breakpoint is a standard concentration for specific antibiotics that determines susceptibility or resistance: MICs below the breakpoint indicate susceptibility and MICs above the breakpoint represent resistance. A document developed by Michigan State University’s Diagnostic Center for Population & Animal Health contains a list of breakpoint values for antibiotics commonly used in animals.5 These values, Dr. Bloom noted, do not change.
Selecting the most appropriate antibiotic requires calculating the efficacy ratio, which can be done as follows:
- From the C/S results, select the antibiotics with MICs reported as “≤ X,” where X is any number.
- Divide the breakpoint by X for each individual antibiotic. The higher the calculated number, the higher the susceptibility will be.
- Rank the antibiotics in order from greatest to least susceptibility.
For example, consider a Staphylococcus bacterial strain that has an MIC of ≤ 1 μg/mL to enrofloxacin (breakpoint = 4) and an MIC of ≤ 4 μg/mL to cephalexin (breakpoint = 32). The efficacy ratio is 4 for enrofloxacin (4/1) and 8 for cephalexin (32/4), indicating that the bacterium is most susceptible to cephalexin. This same calculation can be performed for antibiotics for which the MIC is not reported as “≤ X.”
Calculating this efficacy ratio is particularly important because of the bacterial strain heterogeneity and subsequent antibiotic susceptibility variation within pyoderma skin lesions.
Although the ratio is key to appropriate antibiotic selection, other factors influencing antibiotic selection should be considered, including adverse events, level of tissue penetration, cost, and convenience.
Formularies, Dr. Bloom mentioned, list dose ranges and varying administration frequencies, making it potentially difficult to decide which dose and administration frequency to choose. These recommendations, he explained, are based on susceptibility and the MIC: The closer the MIC is to an antibiotic’s breakpoint, the higher the dose and more frequent the administration needs to be. For empiric antibiotic therapy, the highest listed dose should be used; however, Dr. Bloom warned, this increases cost and the risk of adverse events.

(Top) Pustule and epidermal collarette in a dog with pyoderma. (Bottom) Draining tracts and crusts in a dog with deep pyoderma.
Resistance Genes
Despite a calculated approach to appropriate antibiotic selection for pyoderma treatment, combatting methicillin-resistant Staphylococcus (MRSS, MRSP, MRSA) remains a challenge. Traditionally, clindamycin has been used widely in veterinary medicine for treating Staphylococcus infections. However, S aureus contains 2 inducible genes—msrA and erm—that can mutate spontaneously and confer antibiotic resistance. msrA confers resistance to macrolides (ie, erythromycin), and erm confers resistance to lincosamides (clindamycin and lincomycin).
These resistance-conferring mutations, which occur every 107 to 1010 mutations, are unlikely to show up on C/S testing, though, because of the bacterial concentration used for the tube dilution method; the concentration is not high enough for bacterial replication to produce enough mutations for the resistance-conferring mutations to occur.
This is important because clindamycin resistance may not be observed during C/S testing. For MRSA cases with the msrA mutation, clindamycin resistance may go undetected until after treatment begins. To circumvent this treatment complication when dealing with any methicillin-resistant Staphylococcus for which the culture indicates resistance to erythromycin, Dr. Bloom strongly advised against using clindamycin even if the culture shows susceptibility to clindamycin because the bacteria will likely develop resistance to the medication.
Treating Pyodermas
Topical Therapy
Resistance to systemic antibiotics warrants the use of topical therapies for treating bacterial pyodermas. Topical therapy can reduce or even eliminate the need for systemic antibiotic treatment. However, its use may be limited by an owner’s time constraints as well as cost constraints if the affected skin area is large.
Bathing with shampoos that contain ingredients such as chlorhexidine or benzoyl peroxide is an important topical therapy, Dr. Bloom explained, because doing so gets bacteria off the skin. Which ingredient is the most effective is difficult to determine, though, because of the lack of systematic reviews and randomized double-blinded controlled studies evaluating the ingredients. However, in a review of studies on shampoo therapy, chlorhexidine had the highest evidence of effectiveness, followed by benzoyl peroxide— containing shampoos.
Although 10 to 15 minutes of contact time is typically recommended for baths, there are no studies that justify this recommendation. Notably, a study evaluating bathing with 2% chlorhexidine found that just 1 to 2 minutes of contact time every other day for a week was as effective as 10 minutes every other day.6
Bleach is another effective topical therapy. One option is to use Dakin’s solution, which is commercially available dilute bleach. You can mix it up yourself, daily, using 2 oz of bleach (6%-8%) with 32 oz of water and 0.5 tsp baking soda. Allow a 1- to 2-minute contact time for the shampoo and then rinse. Then bathe the dog with an antimicrobial shampoo and apply a moisturizer.
Because shampoos are not considered a drug, Dr. Bloom advised using high-quality shampoos only from companies that follow Current Good Manufacturing Practices, which are FDA regulations that ensure proper manufacturing.
Clipping is another component of topical therapy, facilitating visualization of the full extent of skin lesions.
When treating SBF with topical antibiotics, treat for either 21 days or 14 days past clinical resolution (as determined by a veterinarian), whichever is longer. Deep pyodermas require at least 6 weeks of treatment or 21 days past clinical resolution, whichever is longer. Regarding glucocorticoids, a 21-day tapering dose of prednisone can be used in SBF if there is intense pruritus and the dog has a fairly localized pyoderma; glucocorticoids should never be used for deep pyodermas.
Systemic Therapy
When discussing systemic antiobiotic therapy for bacterial pyoderma, Dr. Bloom focused on the use of third-generation cephalosporins (cefpodoxime, cefovecin) and fluoroquinolones.
The higher-generation cephalosporins have broad-spectrum activity against gram-negative bacteria. Using broad-spectrum antibiotics in a “go big or go home” approach, though, can select for resistance in nontargeted and nonpathogenic microorganisms; these microorganisms can then spread resistance genes to pathogenic bacteria. In particular, third-generation cephalosporins and fluoroquinolones increase the incidence of extended-spectrum β-lactamase—producing bacteria, which are frequently multidrug resistant.
Not only does the extended-spectrum β-lactamase enzyme have a comparatively broader range of activity than standard β-lactamase enzymes, its resistance spreads through plasmid, widening its distribution among humans and animals.
Given the risk of widespread multidrug resistance, human and veterinary health organizations have developed consensus statements and guidelines regarding the use of higher-generation cephalosporins and fluoroquinolones. For example, Swedish Veterinary Association guidelines state that “third- or fourth-generation cephalosporins should only be used in situations where their use is considered of the utmost importance to the animal’s welfare and where there is a sound basis to suspect that alternative treatments will not have the desired effect.”7 The American College of Veterinary Internal Medicine consensus statement indicates that “limiting use of classes such as the third-generation cephalosporins and fluoroquinolones is widely accepted and consistent with principles of antimicrobial stewardship.”8
On the human side, the World Health Organization has categorized antibiotics as critically important, highly important, or important, according to their usefulness in human health. Among the critically important antibiotics, third- and fourth-generation cephalosporins and fluoroquinolones are further classified as “highest priority.” Moreover, the European Medicines Agency has designated third- and fourth-generation cephalosporins and fluoroquinolones as the most important critically important antibiotics.
Bringing It Together
For treating canine bacterial pyoderma, Dr. Bloom emphasized that veterinarians should be very selective with antibiotics, particularly third- and fourth-generation cephalosporins and fluoroquinolones. As a concluding thought, he said that “we have to look at the impact on human medicine when selecting an antibiotic in veterinary medicine.”
Dr. Pendergrass received her DVM from the Virginia-Maryland College of Veterinary Medicine and completed a postdoctoral fellowship at Emory University’s Yerkes National Primate Research Center. She is the founder and owner of JPen Communications, LLC, a medical communications company.
References:
- Harada K, Okada E, Shimizu T, Kataoka Y, Sawada T, Takahashi T. Antimicrobial resistance, virulence profiles, and phylogenetic groups of fecal Escherichia coli isolates: a comparative analysis between dogs and their owners in Japan. Comp Immunol Microbiol Infect Dis. 2012;35(2):139-44. doi: 10.1016/j.cimid.2011.12.005.
- Manian FA. Asymptomatic nasal carriage of mupirocin-resistant, methicillin-resistant Staphylococcus aureus (MRSA) in a pet dog associated with MRSA infection in household contacts. Clin Infect Dis. 2003;36(2):e26-e28. doi: 10.1086/344772.
- Boost MV, O'Donoghue MM, James A. Prevalence of Staphylococcus aureus carriage among dogs and their owners. Epidemiol Infect. 2008;136(7):953-964. Doi: 10.1017/S0950268807009326.
- Weese JS, van Duijkeren E. Methicillin-resistant Staphylococcus aureus and Staphylococcus pseudintermedius in veterinary medicine. Vet Microbiol. 2010;140(3-4):418-429. doi: 10.1016/j.vetmic.2009.01.039.
- Michigan State University Diagnostic Center for Population & Animal Health. Resistance breakpoints for antimicrobials used in animals. Michigan State University website. https://animalhealth.msu.edu/sections/bacteriology/webcd.bact.ref.011.pdf. Published January 31, 2014. Accessed May 30, 2018.
- Murayama N, Nagata M, Terada Y, et al. Contact time of 2% chlorhexidine acetate for canine superficial pyoderma. Proc North Am Vet Derm Forum. 2011:236.
- Swedish Veterinary Association. Guidelines for the clinical use of antibiotics in the treatment of dogs and cats. Swedish Veterinary Association website. svf.se/Documents/S%C3%A4llskapet/Sm%C3%A5djurssektionen/Policy%20ab%20english%2010b.pdf. Revised 2009. Accessed May 30, 2018.
- Weese JS, Giguère S, Guardabassi L, et al. ACVIM consensus statement on therapeutic antimicrobial use in animals and antimicrobial resistance. J Vet Intern Med. 2015;29(2):487-498. doi: 10.1111/jvim.12562.
