Clinical Signs and Diagnosis of Lyme Disease in Dogs
Lyme disease is among the most frequently diagnosed, zoonotic, tick-borne diseases worldwide and continues to receive intense attention in small animal medicine since canine disease was first reported in the early 1980s.
Lyme disease (borreliosis) is among the most frequently diagnosed, zoonotic, tick-borne diseases worldwide1 and continues to receive intense attention in small animal medicine since canine disease was first reported in the early 1980s.2 In animals, clinical Lyme disease occurs primarily in dogs3 and is most prevalent in New England and along the East Coast, as well in the upper Midwestern and West Coast states (including California).4,5
Infection
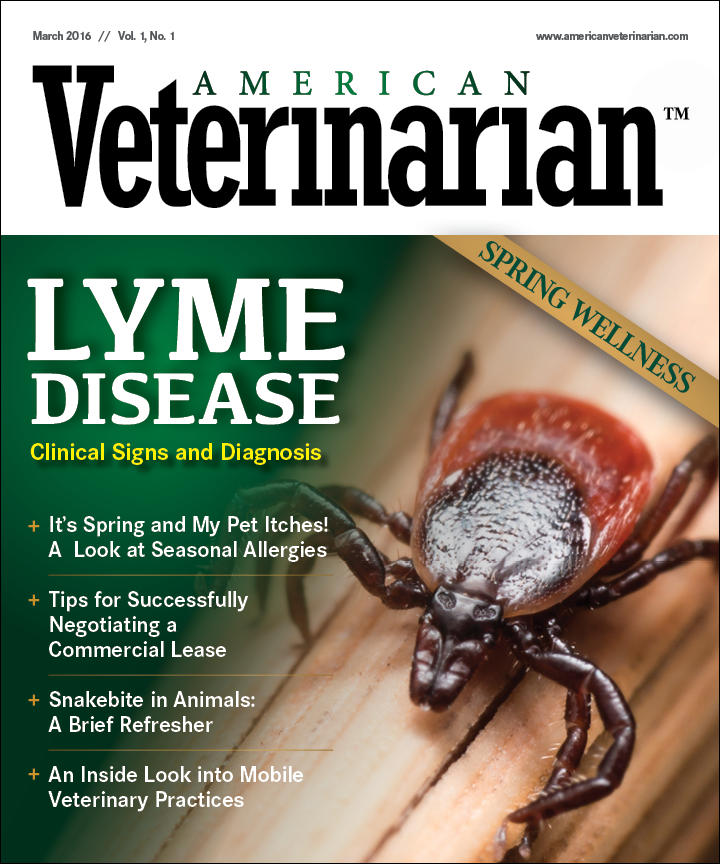
In North America, the disease is caused by the spirochetal bacterium Borrelia burgdorferi sensu stricto,4 which is transmitted by the bite of Ixodes ticks. Ixodes scapularis (the blacklegged tick) is the main vector in eastern and central North America, while Ixodes pacificus (the western blacklegged tick) is the main vector west of the Rocky Mountains.3
Infection of dogs is more common in areas with endemic populations of ticks and where acaricide use is nonroutine; however, infection is rare in dogs in nonendemic areas without a travel history to an endemic area.5 Typically, ticks must attach and feed for 24 to 48 hours before B. burgdorferi transmission occurs.3
Clinical Signs and Disease Manifestations
In dogs, clinical Lyme disease is a less common outcome of infection than in humans, and only about 5% of dogs develop clinical signs of Lyme disease when exposed to B. burgdorferi. Clinical disease usually presents with acute signs such as fever, lethargy, anorexia, depression, lameness, joint swelling, polyarthritis, and/or lymphadenopathy, as well as neuroborreliosis in chronic cases.1 Although uncommon, nephropathy can also occur in advanced stages of the disease.3
Diagnosis
Tests for B. burgdorferi infection detect the presence of either the organism itself or antibodies to it:6
Detection of the organism
Although culture isolation of B. burgdorferi from tissue or blood is the definitive method for diagnosis of infection, this test has low sensitivity, requires incubation periods of up to 6 to 8 weeks, and is usually limited to research settings.2 Detection of the organism by polymerase chain reaction or cytology is also difficult.6
Detection of antibodies to B. burgdorferi
In contrast, serological assays for detection of B. burgdorferi antibodies are highly sensitive and specific, and are widely used in clinical practice to identify B. burgdorferi infection.2 Confirmation of a high titer of B. burgdorferi-specific antibodies has typically involved a 2-step procedure of a quantitative nonspecific enzyme-linked immunosorbent assay (ELISA) followed by qualitative specific Western blotting. Because the nonspecific ELISA measures antibodies to the whole organism and cannot differentiate between antibodies from natural exposure to the organism and vaccination, it produces positive results in both cases and is therefore followed by a confirmatory Western blot test.7
However, more recent confirmatory tests have also emerged, in particular based on C6 detection. Both qualitative (in-clinic test kits) and quantitative (performed in reference laboratories) versions of the C6 test are available. C6 is a peptide associated with the variable region of B. burgdorferi, but only in live organisms, and is immunodominant in dogs infected with B. burgdorferi; it is expressed when the organism is transmitted to the dog, but is not expressed in the tick, in tissue culture, or in Lyme disease vaccines. Antibodies against C6 are therefore highly specific for B. burgdorferi and indicate natural exposure. C6 antibody responses occur 3 to 5 weeks after infection and decline following treatment of dogs with clinical Lyme disease.2,6,7
The qualitative in-clinic test is therefore useful for screening for B. burgdorferi infection, either as part of a screening program for dogs without clinical signs or when Lyme disease is suspected; a positive result indicates active infection with the organism. The quantitative C6 test is effective in measuring response to antibiotic therapy in dogs with Lyme disease, as decreasing levels of the C6 antibody indicate infection control.2,6,7
Fluorescent bead-based multiplex assay of antibodies to B. burgdorferi is a novel and highly sensitive approach for the simultaneous evaluation of antibodies to different B. burgdorferi antigens as indicators of acute or chronic infection. These include outer-surface protein A (OspA), OspC, and OspF that are differentially expressed either in ticks (OspA) during transmission to the host (OspC) or later in the host (OspF). The OspC antibody response is therefore used to indicate early infection and OspF is used for chronic infection.7
It is important to remember that serological test results can be used to document exposure to B. burgdorferi, but not to diagnose Lyme disease. Serological screening of healthy dogs for exposure to B. burgdorferi is therefore controversial because it can lead to overdiagnosis or overtreatment of Lyme disease, although most of these dogs will never develop clinical disease. The consensus opinion of the American College of Veterinary Internal Medicine (ACVIM) is that dogs with proteinuria in endemic areas should be screened for B. burgdorferi exposure with antibody tests. Although the treatment benefit of seropositive healthy dogs remains unknown, ACVIM also recommends that seropositive dogs should be screened for proteinuria and other co-infections and tick control should be initiated.6
In conclusion, a presumptive diagnosis of Lyme disease in dogs must be based on clinical presentation, a history of tick exposure and/or Lyme disease risk, laboratory serological test results, elimination of differential diagnoses, and response to treatment.6
Dr Parry graduated from the University of Liverpool, England in 1997 and is a board-certified veterinary pathologist. After 13 years working in academia, she founded Midwest Veterinary Pathology, LLC where she now works as a private consultant. She is passionate about veterinary education and serves on the Indiana Veterinary Medical Association’s Continuing Education Committee. She regularly writes continuing education articles for veterinary organizations and journals, and has also served on the American College of Veterinary Pathologists’ Examination Committee and Education Committee.
References:
- Chomel B. Lyme disease. Rev Sci Tech. 2015;34(2):569-576.
- Berrada ZL, Telford III SR. Burden of tick-borne infections on American companion animals. Top Companion Anim Med. 2009;24(4):175-181. doi: 10.1053/j.tcam.2009.06.005.
- Bouchard C, Leonard E, Koffi JK, et al. The increasing risk of Lyme disease in Canada. Can Vet J. 2015;56(7):693-699.
- Krupka I, Straubinger RK. Lyme borreliosis in dogs and cats: background, diagnosis, treatment and prevention of infections with Borrelia burgdorferi sensu stricto. Vet Clin North Am Small Anim Pract. 2010;40(6):1103-1119. doi: 10.1016/j.cvsm.2010.07.011.
- Lyme disease. Companion Animal Parasite Council website. http://www.capcvet.org/capc-recommendations/lyme-disease. Published June 2015. Accessed January 5, 2016.
- Littman MP, Goldstein RE, Labato MA, Lappin MR, Moore GE. ACVIM Small Animal Consensus Statement on Lyme Disease in Dogs: Diagnosis, Treatment, and Prevention. J Vet Intern Med. 2006;20(2):422-434.
- Wagner B, Freer H, Rollins A, et al. Antibodies to Borrelia burgdorferi OspA, OspC, OspF, and C6 antigens as markers for early and late infection in Dogs. Clin Vaccine Immunol. 2012;19(4):527-535. doi: 10.1128/CVI.05653-11.