How to Avoid Common Insulin Therapy Errors
Giving proper advice to clients of diabetic pets requires an understanding of the many problems that can result from mistakes made in the choice, use, and monitoring of insulin.

Diabetes mellitus (DM) is a common disorder in dogs and cats. Learning how to care for a pet with diabetes can overwhelm clients, especially those with no prior medical experience. To ensure appropriate patient care and provide clients with the best support and advice, the entire veterinary team should be well informed about the diagnosis and treatment of this disease.
RELATED:
- AAHA Releases Updated Diabetes Guidelines
- Long-Term Efficacy of Gene Therapy for Diabetes Mellitus
Treatment of DM requires attention to detail and a consistent protocol. It is very easy for small errors to creep into a management protocol, leading to poor glycemic control and potentially life-threatening events such as diabetic ketoacidosis and hypoglycemia. An understanding of appropriate protocols and potential treatment errors by the entire team will improve patient care and lead to better outcomes for diabetic patients and their owners.1
DM is caused by an absolute or relative insulin deficiency that results in decreased glucose uptake into cells, increased hepatic glucose production, hyperglycemia, and glucosuria. Type 1 DM, the more common form in dogs, is caused by irreversible loss of beta cell function, whereas type 2 DM results from impaired insulin secretion and insulin resistance and is seen more often in cats. At diagnosis, most cats have type 2 DM, but progressive loss of beta cells may lead to type 1 disease.
Diagnosis of DM relies on identification of characteristic historical and physical examination findings, such as polyuria, polydipsia, polyphagia, and weight loss, together with documentation of hyperglycemia and glycosuria. Detection of serum or urine ketones also supports the diagnosis. In cats, it is particularly important to differentiate stress hyperglycemia from DM. Increased serum fructosamine concentration is suggestive of DM, whereas in stress hyperglycemia, fructosamine is typically within reference range.
Treatment of DM in dogs and cats should include insulin administration, dietary manipulation, obesity management, treatment of concurrent illness, and withdrawal of medications that cause insulin resistance. Insulin treatment is the cornerstone of therapy.
Common Treatment Errors
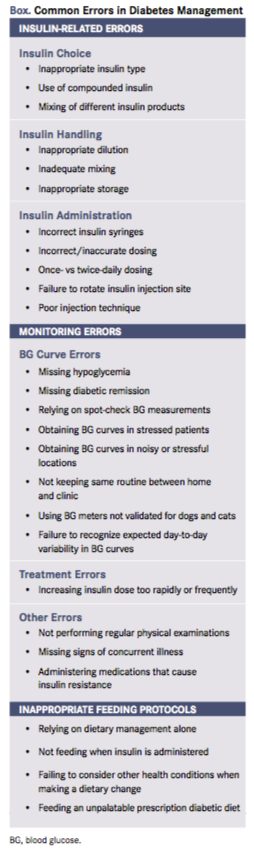
Many common errors can interfere with the response to treatment of a diabetic dog or cat. Common problems include poor insulin choice, errors in insulin handling or administration, errors in monitoring, and inappropriate feeding protocols (Box).
Insulin Choice
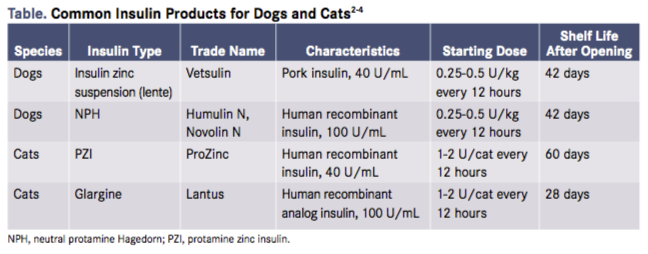
The most common insulin products used for initial management of diabetic dogs and cats are shown in the Table.2-4 Neutral protamine Hagedorn (NPH) insulin is not recommended for diabetic cats because it is very short acting in that species and usually does not result in good glycemic control. Use of compounded insulin products is also not recommended. In a study of compounded protamine zinc insulin (PZI), the authors documented incorrect insulin concentration, incorrect pH, interlot variability in potency, and inappropriate zinc content in insulins purchased from many compounding pharmacies.4 Inappropriate concentrations of free insulin in solution and inappropriate endotoxin concentrations were also documented. These deviations from United States Pharmacopeia guidelines for compounded insulin products have the potential to cause clinically significant adverse effects in diabetic pets.
In dogs, long-acting insulins such as PZI and glargine are not recommended for initial treatment of newly diagnosed diabetic patients; however, these insulins may be useful in select patients with rapid insulin metabolism.
Lastly, it is important to remember that different brands of the same insulin formulation (eg, Humulin N and Novolin N) are not interchangeable because of differences in manufacturing techniques. It is also important to avoid mixing different insulin formulations together.
Insulin Handling
Dilution of insulin products is not recommended as standard practice for most diabetic patients, not only because communication errors can lead to mistakes but also because dilution shortens the insulin’s shelf life. Insulin dilution does, however, make it easier to draw up small volumes of insulin accurately. Unfortunately, most commercial insulin products cannot be diluted because dilution changes critical parameters such as pH, pharmacokinetic properties, and stability of insulin formulations. NPH is the only insulin product that can be diluted with either a commercial diluent or sterile saline, but doing so decreases the stability of the insulin. For small insulin doses, it is preferable to use U40 insulin and syringes or insulin pens with 0.5U markings.
Another important aspect of handling— depending on the type of insulin used—is how to mix insulin prior to administration. Some insulin products such as insulin zinc suspension (Lente) should be shaken thoroughly; others, such as PZI and NPH insulin, should be rolled or inverted gently until fully suspended. Insulin solutions such as glargine do not need to be mixed.
Although most insulin products are stable at room temperature, it is recommended that they are stored in the refrigerator in an upright position. Refrigeration prolongs the shelf life and decreases the likelihood of bacterial growth. Refrigeration is particularly important for clients who—because of both the small insulin doses needed by many patients and the cost of insulin— do not always discard the insulin at the time recommended by the manufacturer.
It is very important to inspect insulin products before each injection. Insulin suspensions such as PZI, Lente, and NPH should be uniformly white and cloudy, with no particulate matter or crystals. Insulin solutions such as glargine should be clear with no particulate matter or crystals present. If abnormalities are noted, the insulin bottle should be discarded and replaced.
Insulin Administration
Because the concentration of insulin products varies, it is very important to use the appropriate insulin syringe for each formulation. If U40 syringes are used to deliver U100 insulin, the insulin dose will be 2.5 times the intended dose, whereas if U100 syringes are used to deliver U40 insulin, the dose will be 2.5 times too low. Adjusting the insulin dose to account for use of incorrect insulin syringes is not recommended because this can lead to serious dosing errors.
Poor administration technique is a common cause of poor response to insulin. Numerous resources, including videos available online, outline the correct technique for insulin injection. Instructions for use of insulin pens are also available online. Owners should be taught proper injection technique and appropriate injection locations by veterinarians or veterinary technicians. If there is any concern about a good response to treatment, the owner’s technique should be reevaluated. Common injection errors include not ejecting air bubbles from the syringe, not priming insulin pens, and not rotating the site of insulin injection.
Most diabetic cats and dogs should be treated with insulin twice daily. Although clinical signs may be controlled using once-daily insulin in some animals, the risk of hypoglycemia is higher and it is less likely that good glycemic control will be achieved.In cats, once-daily insulin treatment may decrease the chance of diabetic remission.
Common Monitoring Errors
Response to insulin treatment should be assessed by evaluation of clinical signs, blood glucose (BG) concentrations, and measurement of urine glucose and fructosamine concentrations. In dogs and cats predisposed to development of ketoacidosis, urine ketones should also be measured. Common errors in insulin monitoring include failing to identify hypoglycemia or diabetic remission,7 increasing the insulin dose too quickly, and relying on spot-check BG measurements alone to adjust insulin therapy.
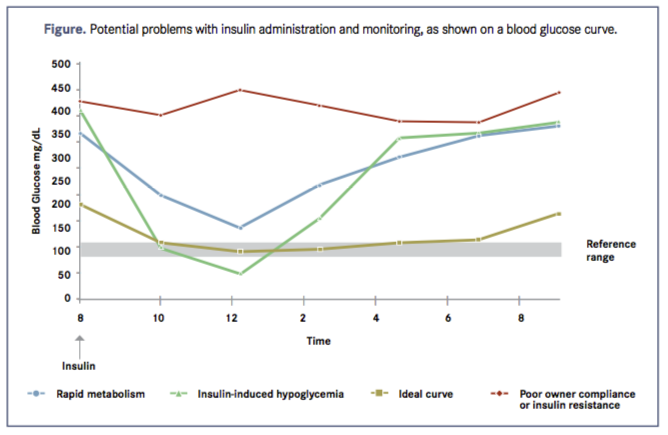
In most patients, BG curves should be performed every 3 to 6 months to adjust insulin dose and detect occult hypoglycemia (Figure). BG curves should also be performed in any diabetic patient with poor control of clinical signs and 10 to 14 days after a dose or formulation change. BG curves are ideally performed using home monitoring but can be performed in the clinic. Day-to-day variability should be expected whether the cat or dog is in the clinic or at home.8
It is very important not to evaluate the pet’s response to insulin until adequate time has elapsed. The insulin dose should not be increased more frequently than every 7 days. If BG is measured in the first few days, the measurement should be used only to detect hypoglycemia. When performing a BG curve, every attempt should be made to minimize the stress of the experience and keep the conditions as similar as possible to a normal day. BG is typically measured every 2 hours for 8 to 12 hours, starting 2 hours after the morning insulin dose and finishing just before the evening dose. In some circumstances, BG measurement every 3 to 4 hours is adequate. Even if the curve is performed in the clinic, it is ideal if the patient is fed and dosed at home prior to arrival. The most important parameters to evaluate when performing a BG curve are the BG nadir and the duration of effect. The BG nadir should be between 80 and 150 mg/dL, and the duration of effect should ideally last 10 to 12 hours (BG <300 mg/dL). It is important to remember that the BG curve should be interpreted in light of the clinical signs, serum fructosamine concentration, and any other information such as urine glucose.
Common Dietary Errors
Low-carbohydrate, high-protein diets are recommended in newly diagnosed diabetic cats,9 while most dogs should be fed high-fiber and low- to moderate-fat diets. Diets for diabetic dogs and cats must be palatable and, if appropriate, calorie restricted to control obesity. It is recommended that the daily portion is divided into 2 meals fed at the time of each insulin injection, although many cats prefer to nibble throughout the day.
Common errors in feeding diabetic dogs and cats include relying on diet alone to control BG in a newly diagnosed diabetic cat, failing to feed at the time of the insulin injection, not taking into account the dietary requirements of other medical conditions, and continuing to feed a prescription diabetic diet that is not palatable. Excessive use of snacks and snacks that contain simple sugars may also cause problems in diabetes control.
Summary
Management of diabetic patients requires attention to detail, and errors may lead to poor diabetic management. Some of the most common errors that lead to poor glycemic control in veterinary patients include failing to account for stress hyperglycemia on a BG curve, missing diabetic remission in cats, and misinterpretation of BG curves in both dogs and cats. Insulin-induced hypoglycemia is also a common cause of poor glycemic control in both dogs and cats.
Dr. Scott-Moncrie, a professor of small animal internal medicine and head of the Department of Veterinary Clinical Sciences at Purdue University, has authored more than 70 peer reviewed publications in small animal endocrinology and internal medicine. Her research and clinical interests are canine and feline endocrinology.
References:
- Behrend E, Holford A, Lathan P, Rucinsky R, Schulman R. 2018 AAHA Diabetes Management Guidelines for dogs and cats. J Am Anim Hosp Assoc. 2018;54(1):1-2 doi: 10.5326/JAAHA-MS-6822. aaha.org/public_documents/guidelines/diabetes%20guidelines_final.pdf. Accessed March 21 2018.
- Nelson RW, Henley K, Cole C. Field safety and efficacy of protamine zinc recombinant insulin for treatment of diabetes mellitus in cats. J Vet Intern Med. 2009;23(4):787-793. doi: 10.1111/j.1939-1676.2009.0342.x.
- Roomp K, Rand J. Intensive blood glucose control is safe and effective in diabetic cats using home monitoring and treatment with glargine. J Feline Med Surg. 2009;11(8):668-682. doi: 10.1016/j.jfms.2009.04.010.
- Monroe WE, Laxton D, Fallin EA, et al. Efficacy and safety of a purified porcine insulin zinc suspension for managing diabetes mellitus in dogs. J Vet Intern Med. 2005;19(5):675-682.
- Palm CA, Boston RC, Refsal KR, Hess RS. An investigation of the action of neutral protamine Hagedorn human analogue insulin in dogs with naturally occurring diabetes mellitus. J Vet Intern Med. 2009;23(1):50-55. doi: 10.1111/j.1939-1676.2008.0249.x.
- Scott-Moncrieff JC, Moore GE, Coe J, Lynn RC, Gwin W, Petzold R. Characteristics of commercially manufactured and compounded protamine zinc insulin. J Am Vet Med Assoc. 2012;240(5):600-605. doi: 10.2460/javma.240.5.600.
- Zini E, Hafner M, Osto M, et al. Predictors of clinical remission in cats with diabetes mellitus. J Vet Intern Med. 2010;24(6):1314-1321. doi: 10.1111/j.1939-1676.2010.0598.x.
- Alt N, Kley S, Haessig M, Reusch CE. Day to day variability of blood glucose concentration curves generated at home in cats with diabetes mellitus. J Am Vet Med Assoc. 2007;230(7):1011-1017. doi: 10.2460/javma.230.7.1011.
- 9. Bennett N, Greco DS, Peterson ME, Kirk C, Mathes M, Fettman MJ. Comparisons of a low carbohydrate-low fiber diet and a moderate carbohydrate-high fiber diet in the management of feline diabetes mellitus. J Feline Med Surg. 2006;8(2):73-84. doi: 10.1016/j.jfms.2005.08.004.
