Clinical Tidbits (April 2018)
Clinical advice and insight from veterinary experts around the country.
Lymph Nodes: When to Aspirate
The most common time veterinarians perform lymph node aspiration is probably when the lymph node is enlarged, according to Anne Barger, DVM, MS, DACVP, clinical professor in pathobiology at the University of Illinois. “So, either on physical exam you palpate 1 or more lymph nodes and notice enlargement, or if a patient is having some sort of abdominal or thoracic imaging the structure is visualized and it’s able to be aspirated,” she says. But the other time to aspirate a lymph node is when the animal has another kind of tumor and you’re worried that it may have traveled or metastasized to the lymph node. “That’s why we say part of the staging process for a tumor is to aspirate the draining lymph nodes,” Dr. Barger says.
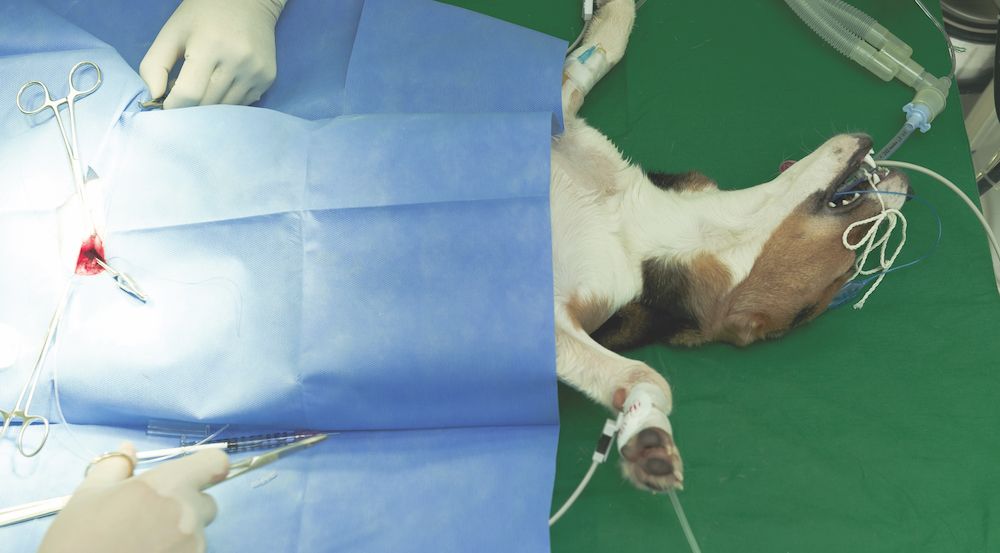
Safer Anesthesia in 2 Steps
The biggest thing we can do to improve safety during anesthetic events, says Khursheed Mama, DVM, DACVAA, professor of veterinary anesthesiology at Colorado State University, is prepare. “Making an anesthetic plan is step 1, so getting a good history, conducting a good physical exam, and doing additional lab work, imaging, and other diagnostics and having all that information when making an anesthetic plan,” she says. Step 2 is calibration. “We need to check our equipment, make sure everything is working, and make sure everything is calibrated,” she says.
Causes of Urinary Incontinence
When we look at urinary incontinence, says Heidi Lobprise, DVM, DAVDC, who practices at Main Street Veterinary Hospital in Flower Mound, Texas, we have to consider conscious and unconscious urinary issues. “If it’s in a very young animal, there could be an ectopic ureter,” she says. “Usually we find it in spayed females that are a little bit older. Large breeds are the most common. As we see this, the sphincter muscle is relaxing, not being able to close tight. And that’s why we have the leakage and the ongoing problems that can occur with it.”
Acute Onset of Neurologic Signs? Think Toxins
“When a young animal is perfectly healthy, and then all of a sudden it’s sick, it can be a medical disease,” says Ken Drobatz, DVM, MSCE, DACVIM, DACVECC, professor of critical care at the University of Pennsylvania, “but I always wonder about toxins.” This is especially true with acute-onset neurologic signs, he says, such as ataxia, wobbliness, altered mentation, and the like. Of course, he notes, you must talk extensively with the pet owner to get to the bottom of things.

Unique Aspects of the Avian Gastrointestinal System
Most psittacine species have a segment of their esophagus called the crop, which is a sac-like area where food can accumulate, says Jennifer Graham, DVM, DABVP (Avian & Exotic Companion Mammal Practice), associate professor of zoological animal medicine at the Cummings School of Veterinary Medicine at Tufts University. “So, if they have any sort of motility issue, they can present with crop distention,” she says. Also, instead of a true stomach, birds have a proventriculus and a ventriculus. Depending on the type of bird, there can be a lot of differences in terms of that as well as the cecal anatomy.
Most clinically relevant, Dr. Graham says, is that birds have a cloaca, which is the common opening of the gastrointestinal, urinary, and reproductive tracts. “If a bird has pathology, such as passing blood in the stool, that could be originating from any one of those systems.”
Where Antimicrobial Resistance Develops
Jill Maddison, BVSc, PhD, FACVSc, SFHEA, MRCVS, professor of general practice in clinical sciences and services at the Royal Veterinary College, says that although it’s commonly believed that antibacterial resistance develops at the site of infection— and sometimes it can be if the infection hasn’t been treated appropriately—other causes are sometimes overlooked. “Whenever we give an antimicrobial,” Dr. Maddison says, “we are affecting the normal flora in the patient.” That normal flora lives in the skin and, importantly, in the gut. “Particularly if we give oral antibiotics, we’re going to be changing the gut flora, which is something we’ve always known. The issue of it causing bacterial resistance, or populations of resistance, or causing the bacterial population to potentially develop dysbiosis, is a more recent understanding that’s come out of research studies,” she says.
Handling Fearful or Aggressive Cats
The single favorite thing Alison Gottlieb, BS, CVT, VTS (ECC), intensive care nurse and education coordinator for CARES (Center for Animal Referral and Emergency Services) in Langhorne, Pennsylvania, likes to use when dealing with fearful or aggressive cats is gabapentin. “Giving a cat 100 mg of gabapentin 2 hours before the visit is life changing for everyone involved,” she says. “The other things I like to use are towels and lots of catnip.”

It’s the perennial problem: Are animals painful or not? Perioperative pain and chronic pain pose different challenges, says James Gaynor, DVM, DACVA, DACVPM, pain specialist at Peak Performance Veterinary Group in Frisco, Colorado. “In the hospital, cats and dogs are really good at hiding their behavioral manifestations of pain, which means either the veterinarian needs to make an assumption about what is painful or we really need to palpate the animal,” he says.
For arthritis pain, owners can help. “They can really tell us whether the dog has had changes in behavior or activity, which are indicative of pain,” he says, “and as we treat them and their behavior and activity return to normal, then they are typi- cally less painful.”

UN, WHO address public health concern over avian flu transmission to humans
April 18th 2024Veterinary professionals working with certain animals are advised to take precautionary steps to minimize risk of infection, while researchers in Texas study potential H5N1 vaccines, antivirals, and antibody therapies for humans
Read More