AVMA 2017: Anesthesia Monitoring With Capnography
Presenting at the 2017 AVMA Convention, Heidi Reuss-Lamky discussed the ways in which capnography provides important feedback about the severity of a patient’s condition and how patients respond to treatment.

Capnography is an essential tool for monitoring anesthetized and critical care veterinary patients, according to Heidi Reuss-Lamky, LVT, VTS (Anesthesia & Analgesia), from Oakland Veterinary Referral Services in Bloomfield Hills, Michigan. Presenting at the 2017 American Veterinary Medical Association Convention in Indianapolis, Indiana, Reuss-Lamky discussed the ways in which capnography provides important feedback about the severity of a patient’s condition and how patients respond to treatment.
Capnography refers to the measurement of CO2 in a patient’s exhaled breath, she said. The measurements are displayed as a capnogram, which is a graphic representation of exhaled CO2 as each breath is taken over time.
Reuss-Lamky highlighted the critical role of this tool in anesthetic monitoring by discussing findings from a key study from the human medical literature of more than 1000 anesthetic-related malpractice claims.1 Anesthesiologist reviewers analyzed the cases and concluded that “using capnography and pulse oximetry together could have prevented 93% of the anesthetic mishaps,” she said.
Key Aspects of Physiology
According to Reuss-Lamky,3 physiologic processes are essential for capnography use and interpretation: metabolism, circulation, and ventilation. Gas exchange occurs in alveolar capillary beds in the lung, she said. CO2 is produced in the body as a byproduct of tissue metabolism, transported to the lungs via perfusion, and then removed via alveolar ventilation. The exhaled CO2 is also known as end-tidal CO2 (ETCO2) and represents the concentration of CO2 in the lung alveoli that emptied last.
RELATED:
- Genetic Cause Found for Acute Respiratory Distress Syndrome in Dalmatians
- Differentiating Between Types of Respiratory Distress in Cats
She explained that CO2 is transported in the body predominantly in 3 forms: 60% to 70% as bicarbonate ions, 20% to 30% bound to proteins, and 5% to 10% dissolved in arterial plasma. Bloodgas analysis measures the CO2 that is dissolved in plasma, said Reuss-Lamky, and this is known as the arterial partial pressure of CO2 (PaCO2).
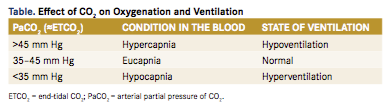
She noted that, in a healthy patient, ETCO2 (normally 35-45 mm Hg) typically correlates with PaCO2 (Table) and is approximately 2 to 5 mm Hg lower. Because this gradient is considered clinically insignificant, she added that ETCO2, PaCO2, and alveolar CO2 (PACO2) levels are considered approximately equal.
Ideally, alveolar ventilation is matched to alveolar perfusion. Under normal conditions in the lung, the ratio of pulmonary ventilation to perfusion is close to 1. However, ventilation—perfusion mismatching may occur in some conditions, leading to abnormal ETCO2 levels (Table).
Why Use Capnography?
Capnography offers many benefits, said Reuss-Lamky. It allows noninvasive assessment of the patient’s systemic metabolism (acid-base status), pulmonary perfusion, and cardiac output.
Because ETCO2 , PaCO2 , and PACO2 levels are considered approximately equal, monitoring ETCO2 levels can help clinicians to detect trends or sudden changes in a patient’s PaCO2. Various clinical conditions, even anesthetic mishaps, may increase the gradient between ETCO2 and PaCO2, such that it becomes clinically significant, she said.
ETCO2 analysis can help evaluate a patient’s acid-base status, respiratory patterns, and adequacy of ventilation in a variety of clinical situations, said Reuss-Lamky. These include during anesthesia when anesthetic drugs and inhalants can reduce tidal volumes significantly, or during long-term ventilatory assistance, such as when a mechanical ventilator is used. Capnography can also help clinicians promptly identify airway mishaps, she added. One example comprises cases in which the endotracheal tube is placed in the esophagus instead of the trachea.
By monitoring ETCO2 using capnography, Reuss-Lamky explained that clinicians can identify and promptly respond to such conditions. For example, ETCO2 levels greater than 45 mm Hg in a patient indicate inadequate ventilation (Table), she said, requiring clinicians to provide ventilatory assistance via manual or mechanical means. Hypoventilation may occur in such condi- tions as pneumothorax or lung disease, she added.
Using capnography also helps clinicians maintain a stable plane of anesthesia. This can be especially useful in obese animals, during prolonged surgical procedures (>90 minutes), or when neuromuscular blocking agents are used. A sudden decrease in ETCO2 can also be an early and reliable indicator of impending cardiovascular collapse or cardiac arrest, she said. Types of Capnography
Two types of capnographs are available, said Reuss-Lamky: mainstream and sidestream devices.
Mainstream Devices
Mainstream, or nondiverting, devices analyze the respiratory gases locally (at the interface between the endotracheal tube and breathing circuit) and provide instant (<100 ms) results. Samples of the patient’s exhaled gases are obtained from the anesthetic circuit using an adapter that attaches to the end of the endotracheal tube. This adapter should be attached at the point of the patient’s nose to avoid excessive dead space and prevent rebreathing of CO2, said Reuss-Lamky.
Mainstream technology is subject to fewer problems secondary to secretions or moisture compared with sidestream devices, involves fewer disposable supplies, and does not require scavenging of sampled waste anesthetic gases, she said. However, mainstream monitors have several disadvantages. Because of their weight and location, they are prone to accidental disconnection, leaks, and damage, and they may cause kinking of the endotracheal tube.
Sidestream Devices
Sidestream, or diverting, devices extract a sample of respiratory gases via tubing into a measurement chamber for analysis and can also be used in patients that are not intubated. These monitors use small, lightweight sensing tees attached at the interface between the endotracheal tube and breathing system. They are also useful for remote monitoring (such as during magnetic resonance imaging).
Sidestream devices, however, have some disadvantages. In small patients, high fresh gas flow rates may produce falsely low ETCO2 readings and waveform changes as a result of sample dilution. Sidestream monitors also have a 2- to 3-second delay in response time and require periodic calibration and replacement of disposable supplies (such as sensing tees). Sampling tubes may become occluded due to buildup of respiratory moisture. This technology also requires scavenging of sampled waste anesthetic gases.
The Capnogram
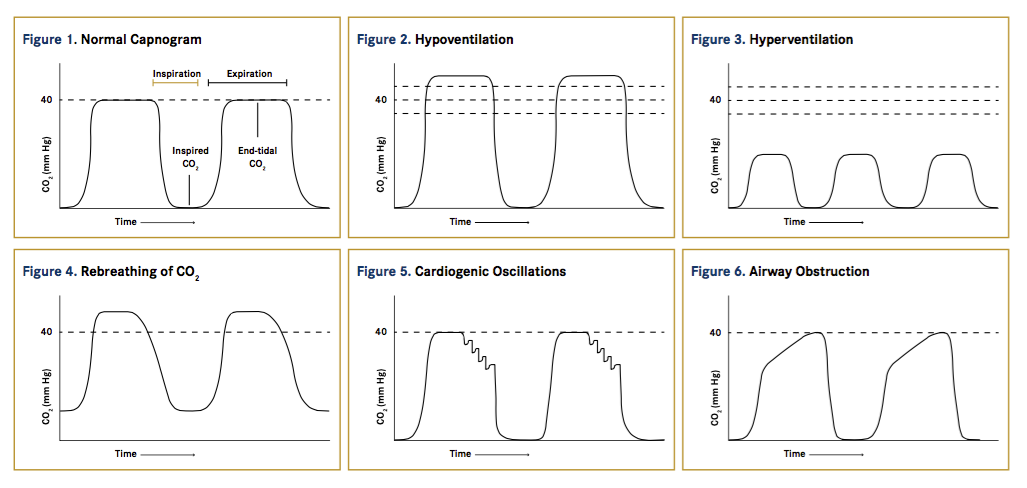
The waveform of the capnogram represents the changes in a patient’s ETCO2 levels over time, said Reuss-Lamky. The upward slope and the top of the waveform represent the exhalation phase, and the downward slope and the bottom of the waveform represent the inhalation phase.
In a normal capnogram (Figure 1) the baseline of the waveform should reach a zero level because the patient should not be inhaling CO2 , the expiratory upstroke of the wave should be steep, the expiratory plateau should be relatively flat, and the inspiratory downstroke should be an almost vertical drop to baseline. The highest point of the plateau represents the actual ETCO2 value. The shape of the capnogram waveform can help clinicians identify problems with the patient’s ventilation, perfusion, or metabolism.
Some Common Abnormal Capnograms
ETCO2 Level Abnormalities
Increased ETCO2 levels (>45 mm Hg) may occur as a result of hypoventilation (Figure 2). This may be due to problems such as airway obstruction, pneumothorax, lung disease, or acutely increased metabolism (eg, in malignant hyperthermia). Decreased ETCO2 levels (<35 mm Hg) may occur as a result of hyperventilation (Figure 3). This may be due to problems such as airway occlusion, endotracheal tube dislodgement, or cardiac arrest.
Other Abnormalities
If the baseline does not return to zero during inspiration, this indicates that the patient is rebreathing exhaled CO2 (Figure 4). Possible causes include an exhausted soda lime absorber or faulty valves in the breathing circuit.
A ripple effect at the end of the expiratory phase represents cardiogenic oscillations as the heart contracts and relaxes against the diaphragm when the lungs are nearly deflated (Figure 5). Cardiogenic oscillations may be seen at low respiratory rates and are considered physiologically insignificant.
A notch (curare cleft) in the top of the waveform in the expiratory plateau may be seen in cases when a patient is receiving a neuromuscular blocking agent and is being ventilated mechanically. These notches indicate that the effect of the neuromuscular blocking agent is wearing off.
A waveform that shows an elevation, or peak, at the end of exhalation just before inhalation—often described as a “shark fin” because of its distinct shape—indicates an airway obstruction (Figure 6). This may be due to such problems as kinks or mucus plugs in the endotracheal tube.
A weak inhalation phase showing decreasing ETCO2 with loss of the expiratory plateau indicates an endotracheal tube cuff leak or deflated cuff.
Conclusion
Capnography represents a valuable tool to help clinicians evaluate and monitor anesthetized veterinary patients. By familiarizing themselves with the waveform of the normal capnogram, clinicians can learn to recognize abnormal waveforms and thus identify underlying clinical situations or technical problems that may affect a patient during anesthesia.
Dr. Parry, a board-certified veterinary pathologist, graduated from the University of Liverpool in 1997. After 13 years in academia, she founded Midwest Veterinary Pathology, LLC, where she now works as a private consultant. Dr. Parry writes regularly for veterinary organizations and publications.
Reference:
- Tinker JH, Dull DL, Caplan RA, Ward RJ, Cheney FW. Role of monitoring devices in prevention of anesthetic mishaps: a closed claims analysis. Anesthesiology. 1989;71(4):541-546.
