Feline Euthanasia - Part 2: Clinical Considerations and Technical Recommendations
Whether the procedure is performed in the clinic or at home, the veterinary team should always have the cat’s mental health and physical comfort and the owner’s feelings top of mind.

A good death requires humane technique. If a cat’s life is to be taken, it should be done with the highest degree of respect and with a singular emphasis on making death as painless and stress-free as possible. The technique employed should result in rapid loss of consciousness followed quickly by cardiac and respiratory arrest and, ultimately, loss of brain function.
Preparations must be complete before the client and patient enter the room, and participants should be instructed to behave in a compassionate manner. Soft voices, slow and gentle movements, and an emphasis on the environment are paramount. The person assisting the doctor should know to leave the room as soon as his or her presence is no longer essential.
The Euthanasia Procedure
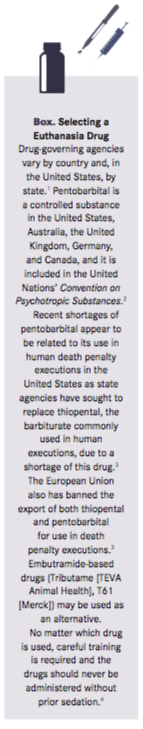
Intravenous (IV) administration of barbiturates, either alone or in combination with other drugs, is the preferred method of euthanasia, and sodium pentobarbital, which produces rapid death, is the preferred drug (Box).1-5 Premedication to provide anxiolysis and analgesia/anesthesia is recommended in all euthanasia procedures.
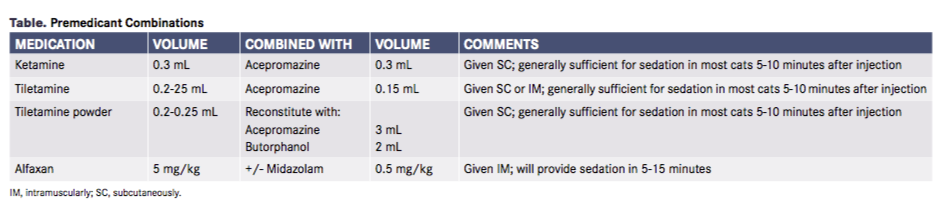
Many humane and relatively painless premedicants and premedicant/anesthetic combinations are available (Table). Choices should be based on staff training, knowledge, and experience with pharmaceuticals commonly used in the veterinary practice. When possible, premedications should be given subcutaneously to avoid discomfort. Diluting the drug with warm sterile water for injection can reduce distress.
If routes other than IV administration are necessary (eg, because a cat is very small, debilitated, or dehydrated), the cat should be fully unconscious or anesthetized. Pentobarbital and secobarbital do not cause tissue irritation, but pentobarbital combination products, such as pentobarbital/phenytoin (eg, Euthasol, Virbac), do. Intraperitoneal administration of a nonirritating barbiturate may be necessary or desirable under certain circumstances.
RELATED:
- Inappropriate Behavior: Leading Cause for Euthanasia
- Thinking Outside the Box with Euthanasia
Recent data on 131 cats euthanized at home demonstrated that intrarenal administration of pentobarbital causes pain-free death very rapidly in the sedated cat.6 The average time to cardiopulmonary arrest was less than 1 minute, and 95% of cats had no observable reaction (agonal breathing, twitching) when 3 to 6 mL of euthanasia solution was given via a 1-inch, 18-gauge needle aimed at the renal cortex. Palpable kidney swelling was used as an indicator of correct administration, although this was not always present. Kidney size, patient weight, and hydration status had no impact on efficacy.6
In-Clinic Euthanasia
Client Communication
As discussed in Part 1 of this series, quality-of-life discussions should take place long before the decision to euthanize is made.7 Then, once the decision has been made, clients need to determine whether to be present for the entire procedure.
Owners who wish to be present should be asked whether they have ever witnessed euthanasia. If the answer is yes, then a brief description of what to expect may suffice. For clients who have never witnessed euthanasia, the veterinarian should detail the procedure in an empathetic manner.
Any potentially upsetting behavior by the cat, such as loss of bladder or bowel control, agonal breathing, or muscle fasciculations, should be described in advance and the owner assured that these signs do not indicate pain or discomfort. The length of time the procedure will take and the steps that will be taken should be described, emphasizing that the cat will be painless. The paramount message should always be that the heartbreaking decision to euthanize was made out of an unselfish and loving desire to prevent their beloved cat from further suffering.
The veterinary team may be the only support the owner has if friends and family do not understand the client’s depth of the attachment to the animal. Compassionate listening and reflecting back to owners an understanding of the intensity of their grief are critical to preserving the veterinarian—client relationship.
Procedure Location
The euthanasia location should be quiet, with good light- ing, adequate ventilation, and little traffic. All the necessary drugs and supplies should be assembled before the owner and pet arrive. During the time between sedative administration and injection of euthanasia solution, owners may welcome a few minutes alone to say goodbye. Their wishes should preempt any concerns about time or schedule. A sign or symbol in the treatment room indicating that a euthanasia is about to be performed can signal staff to maintain quiet and respect. Some practices light a candle in the waiting area to indicate that this procedure is taking place.
Reducing Anxiety and Fear
The anxiety experienced by cats and their owners when cats are taken into the treatment room, or “back” of the hospital, has been well described. At no other time is it more important to be aware of this than when euthanasia is about to be performed. Some things to consider:
- Never take the cat from the owner.
- Many of these cats suffer from multiple or chronic illnesses that may exacerbate the pain response (ie, allodynia, hyperalgesia). Therefore, if IV administration of the euthanasia solution is planned and an IV catheter is not already in place, venous access should be via syringe. IV catheter placement is unpleasant enough in healthy patients without the use of transdermal analgesia.
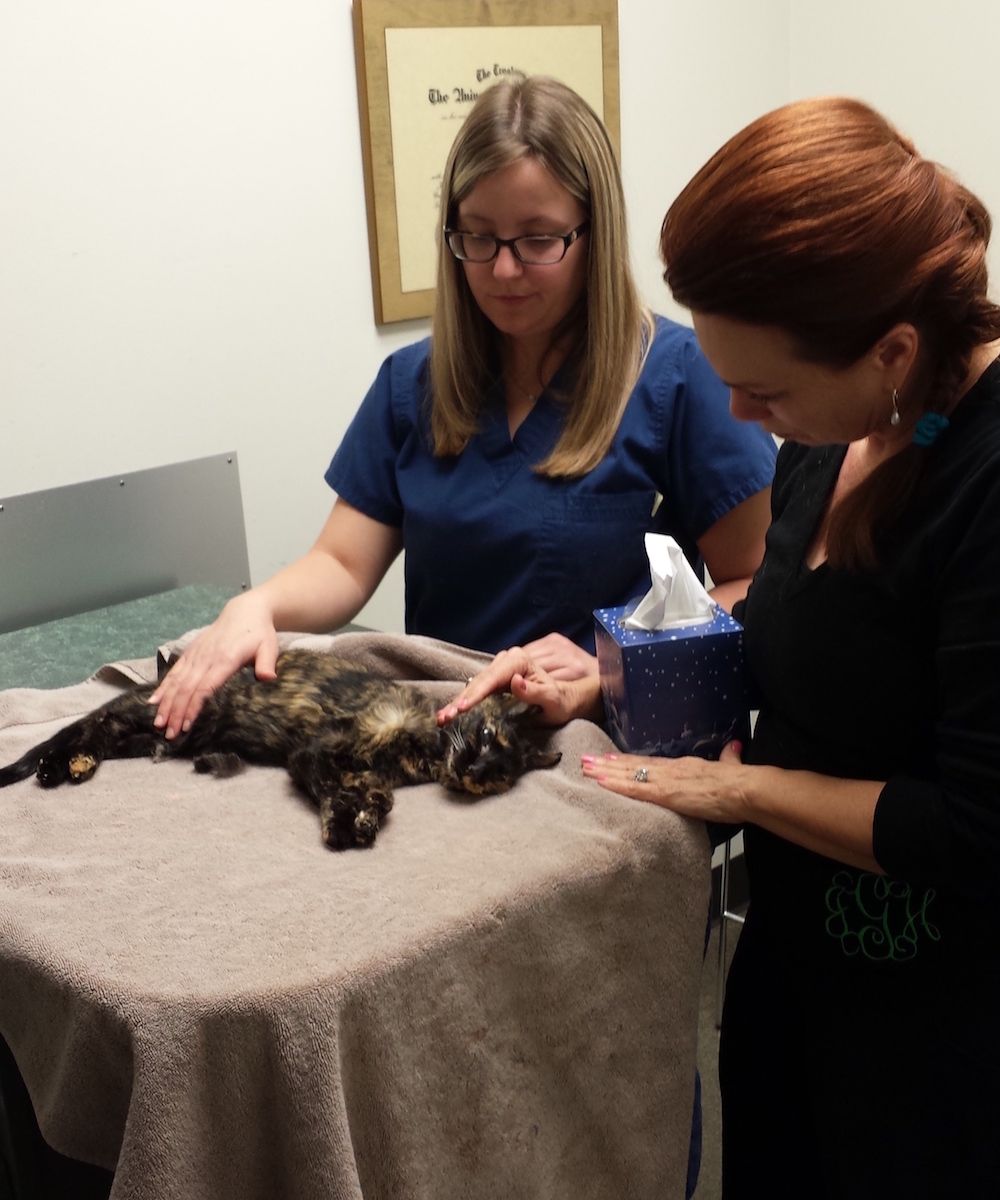
Although the veterinarian should choose the site of IV administration based on skill and experience, the medial saphenous vein has some significant advantages, including clear visibility, easy accessibility, and distance from the patient’s head. If this vein is selected, the euthanasia solution should be diluted and a 25-gauge needle used for injection. If the intraperitoneal route is necessary, the drug can be injected and the cat wrapped in bedding or towels and returned to sit on the owner’s lap. This allows the owner to stroke and speak to the cat and removes the clinical nature of the experience.
- Pay careful attention to the patient’s comfort. The cat can be wrapped in comfortable bedding with only the rear leg left exposed. Injection in this location may negate the need to use clippers, which can be distressing to the cat.
- Bedding or soft towels may also be used to block the visual experience of the procedure for the caregiver. Owners can then be invited to come close to their beloved cat’s face to pet and comfort. Not only does this offer a sense of closeness and connection, but it may help to distract the owner from the technical process.
Confirmation of Death
Armed with a stethoscope, the veterinarian must ensure the cat is deceased following the procedure. This official pronouncement is a vital part of the procedure and provides some closure and allows owners to move from anticipatory to actual grief. At this moment, the relationship the veterinarian has with the owner should guide behavior. Owners should be reminded at this time that they made a loving and compassionate decision. Some people are comforted by a hug; others wish to be left alone with their beloved pet for a while. Care should be taken to accommodate their wishes.
The actions of the veterinarian and staff at this time will influence the client’s final memory of the cat and the experience. Gentle handling and common courtesy are key. If there is concern about the emotional state of the owners, they should be invited to stay for as long as necessary or to contact someone to be with them. Thoughtful inquiry will help provide the support they need.
Final Care and Follow-up
Long before euthanasia is imminent and before powerful emotions come into play, a discussion about aftercare of the body should take place. Final care and disposition of the body must adhere to local, state, and federal laws. If the owner wishes to bury the body at home (and home burial is allowed by law), provision of a cardboard “coffin” can be helpful. Licensed cremation services are widely available and a popular choice for cat owners. If cremation is elected, the choice of return of ashes or group cremation must be recorded and executed.
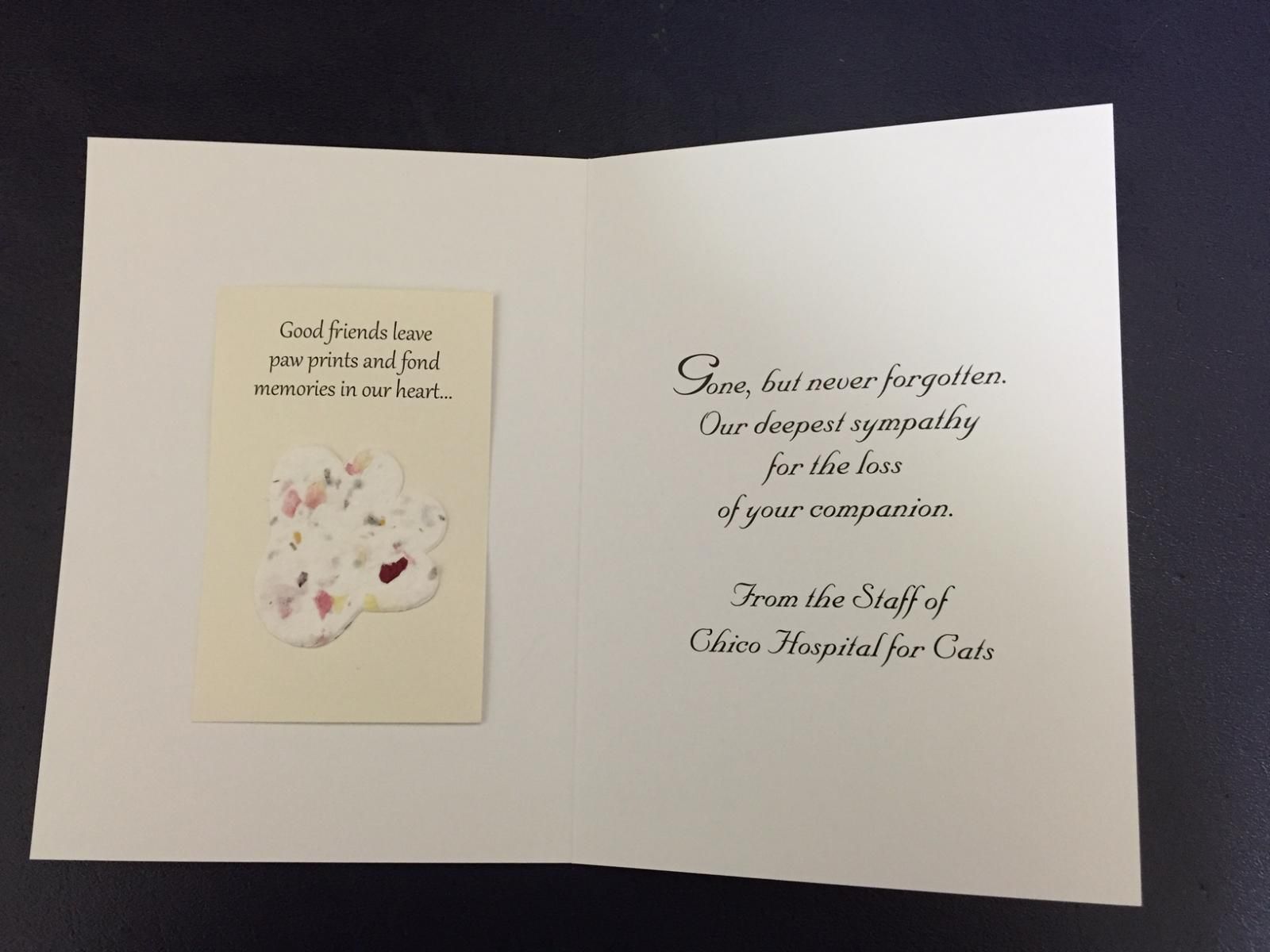
Acknowledgment of the loss of a beloved cat is greatly appreciated by most clients. Personalization is critical. Cards signed by the entire staff, ideally with a personal note from the veterinarian, can help with the grieving process. Many companies create tasteful sympathy cards and memorials. Condolences should always be sent before the invoice. A contribution in the pet’s name might be made to a designated pet memorial program, such as the Winn Feline Foundation. These foundations typically send a condolence card to the client indicating that a contribution has been made by the hospital to honor their cat.
Many grief counseling groups, therapists, and pet loss hotlines exist.8 Owners who are experiencing overwhelming grief should be told about these services. Some grief experts believe that having another pet to nurture helps to end the grieving process, and hospitals can often facilitate this. While some may see this as a betrayal of their lost cat and resist, others will welcome having a new pet to care for and an opportunity to recover from the emptiness they are feeling. In every case, a good sense of timing and respectful acknowledgment of the loss are important.
At-Home Euthanasia
An increasing number of veterinary services, ranging from nationwide franchises (eg, Pet Loss At Home, Lap of Love) to local mobile practices, offer in-home euthanasia. The growth and popularity of these unique veterinary practices reflect what many pet owners today consider valuable and important.9
Advantages
private experience for both themselves and their pet.10 Given how challenging it is to bring some cats into the clinic when they are healthy, it is easy to understand why many owners seek an alternative. The last thing they want is for their pet to experience any level of distress, anxiety, fear, or discomfort at the very end of life.
The primary advantage of at-home euthanasia is that it allows the cat to be comfortable and calm within the familiar smells, furniture, and people of its own environment. Understanding that losing their companion is as painful and difficult as losing a human family member makes at-home euthanasia a very natural and obvious choice for some pet owners.10
At-home euthanasia is as much about the own-ers’ experience as it is about the patient’s. Owners are looking for a private, ceremonial way to say a very peaceful and gentle goodbye.10 Many prefer to experience this grief in the comfort of their home. They can have as many people present as they want without being limited by the size of an exam room or grieving room. There is also flexibility in where the euthanasia is performed, be it in a favorite room or bed, outside in the yard, or on a porch.
Challenges
Even with its many benefits, veterinarians should discuss the drawbacks of at-home euthanasia with pet owners. There is the potential for the room where the euthanasia takes place to become a trigger for sadness for the owner. That visual image and memory of the loss of their companion can prompt owners into cycling through the grief stages long after the event. Additionally, because the cost of in-home euthanasia is typically 2 to 3 times higher than having the procedure performed at the clinic, it may not be an option for some families.
There can be challenges to performing at-home euthanasia for veterinarians as well. They must be able to enter the home and remain focused on the patient and caregiver. This can prove challenging if the home has distractions such as other pets, poor lighting, or tight quarters. Patients also may be fractious, which can make administering a sedative difficult. Traveling to the client’s home can also be challenging depending on weather and traffic conditions.
Finally, at-home euthanasia may bring an extra element of unpredictability. The veterinarian must be prepared if the patient does not react predictably to the sedation protocol. The best way to man-age this unexpected response is to always have a backup plan.10 As mentioned earlier, a very effective and gentle way to perform euthanasia is to start with an anesthetic induction agent to allow the patient to become unconscious, and then proceed with the intrarenal technique for the barbiturate.5,10 If the patient does not achieve an appropriate unconscious state, rendering an intrarenal injection impossible, then the veterinarian must be prepared to change techniques or give additional sedation. This means having the tools, skill, and sufficient medications needed to perform the euthanasia via an IV route.
It is also extremely helpful to have an experienced technician assist with the process and help manage the unexpected. This not only makes dealing with an aggressive patient easier, but it allows the veterinarian to focus on the patient and owner the entire time.
William Ray Folger, DVM, MS, DABVP (Feline Practice) Dr. Folger is the founder and director of Memorial Cat Hospital in Houston, Texas. He has served as the Feline Regent for the American Board of Veterinary Practitioners since 2011.
Elizabeth Colleran, DVM, MS, DABVP (Feline Practice) Dr. Colleran is the founder and director of Chico Hospital for Cats in Chico, California and Cat Hospital of Portland in Portland, Oregon. She is the chair of the Cat-Friendly Practice Committee for the American Association of Feline Practitioners.
TIina Han, DVM Dr. Han is the owner of My Doorstep Vet, PLLC, a house call practice in Houston, Texas, that offers in-home euthanasia and other veterinary services.
Elizabeth Strand, MSSW, PhD Dr. Strand is a clinical associate professor and director of veterinary social work at the University of Tennessee College of Veterinary Medicine in Knoxville. She serves in the American Association of Veterinary Medical Colleges Veterinarian Wellness Awareness Working Group.
References:
- Mid-level practitioners authorization by state. US Department of Justice, Drug Enforcement Administration, Diversion Control Division website. https://www.deadiversion.usdoj.gov/drugreg/practioners/mlp_by_state.pdf#search=pentobarbital. Updated October 13, 2017. Accessed November 13, 2017.
- United Nations Convention on Psychotropic Substances. Final act of the United Nations Conference for the adoption of a protocol on psychotrophic substances. UN Office on Drugs and Crime website. unodc.org/pdf/convention_1971_en.pdf. Published 1971. Accessed November 2, 2017.
- Horne J. Lethal injection drug shortage. The Council of State Governments website. csg.org/pubs/capitolideas/enews/issue65_4.aspx. Published July 2017. Accessed November 2, 2017.
- Gibson J, Lain CB. Death penalty drugs and the international moral marketplace. Georgetown Law J. 2015;103(5): 1215-1274.
- American Veterinary Medical Association. AVMA guidelines for the euthanasia of animals: 2013 edition. AVMA website. avma.org/kb/policies/documents/euthanasia.pdf. Published 2013. Accessed November 2, 2017.
- American Veterinary Medical Association. Animal Welfare Symposium 2014: humane endings - in search of best practices for the euthanasia, humane slaughter and depopulation of animals. AVMA website. avma.org/Events/Symposiums/Pages/2014-Humane-Endings-Symposium.aspx. Accessed November 2, 2017.
- Folger WR, Colleran E, Tina T, Strand E. Feline euthanasia—Part 1: ethics, Aesculapian authority, and moral stress. Am Vet. 2017;2(5):1,XX-XX.
- Bereavement resources. Pet Loss Help website. petlosshelp.org/bereavementresources.html. Accessed November 2, 2017.
- Gregersen S. Giving your clients the best end-of-life experience with their pets. Vet Nurs J. 2016;31(8):241-244. doi: 10.1080/17415349.2016.1197522
- Kahler SC. The end-all practice: home euthanasia. JAVMA. 2015;246(1):14-16.
